TRANSFORMATIVE BUSINESS INTELLIGENCE TO REVOLUTIONIZE REVENUE CYCLE
Transformative Business Intelligence to Revolutionize Revenue Cycle

“Technology is the cornerstone of our organization. Our EOS™ transformative technologies support both people and process, helping us better manage data collection, enhance patient interaction and streamline the eligibility process from program identification to application approvals, denial management, disability and insurance recover needs. Invicta’s Business Intelligence prowess is a differentiator that cannot be ignored – it allows us to remove inefficiencies, deploy staff where they are most valuable and produce superior results.”
– Donny Zamora, Chief Executive Officer
“Technology is the cornerstone of our organization. Our EOS™ transformative technologies support both people and process, helping us better manage data collection, enhance patient interaction and streamline the eligibility process from program identification to application approvals, denial management, disability and insurance recover needs. Invicta’s Business Intelligence prowess is a differentiator that cannot be ignored – it allows us to remove inefficiencies, deploy staff where they are most valuable and produce superior results.”
– Donny Zamora, Chief Executive Officer
Table of Contents
Our experts have created standardized metrics designed to provide concierge level service to our clients, streamline processes and outperform traditional revenue cycle management solutions.
Our experts have created standardized metrics designed to provide concierge level service to our clients, streamline processes and outperform traditional revenue cycle management solutions.
The use of cognitive technology to automate business processes has become the most important factor in evaluating an effective revenue cycle operation. The systemic redesign of traditional revenue cycle workflows is necessary to ensure that humans and machines augment each other’s strengths and overcome individual weakness. We understand this transformation does not happen overnight. Invicta’s EOS™ suite of technology solutions are designed to create an incremental roadmap of improvement while capturing key analytics that can be used to drive future change.
Invicta maintains a fully integrated workflow and data management system that breaks down traditional revenue cycle inter-departmental barriers. The robust platform provides greater accountability for patient tracking and metrics by providing real time data. The Invicta EOS™ platform automates the many moving parts of a patient account and has extensive experience interfacing with all major hospital systems. From referral to confirmation of payment, the system allows us to follow an account all the way through reimbursement while improving payer and patient engagement.
The use of cognitive technology to automate business processes has become the most important factor in evaluating an effective revenue cycle operation. The systemic redesign of traditional revenue cycle workflows is necessary to ensure that humans and machines augment each other’s strengths and overcome individual weakness. We understand this transformation does not happen overnight. Invicta’s EOS™ suite of technology solutions are designed to create an incremental roadmap of improvement while capturing key analytics that can be used to drive future change.
Invicta maintains a fully integrated workflow and data management system that breaks down traditional revenue cycle inter-departmental barriers. The robust platform provides greater accountability for patient tracking and metrics by providing real time data. The Invicta EOS™ platform automates the many moving parts of a patient account and has extensive experience interfacing with all major hospital systems. From referral to confirmation of payment, the system allows us to follow an account all the way through reimbursement while improving payer and patient engagement.
- Real-time API or batch connectivity
- “Next Day” turn around response time for batches
- Flexible file exchange workflows for batch connectivity
- Complete the work overnight with viable responses to you the following morning
- File exchange delivery via custom-built SFTP just for you
- No tedious payer credentialing requirements – a simple one-page signed authorization form is all we need
- Add a custom field to your return file to facilitate automation or workflows for your internal workflow management system
- Crosswalk your EPIC billing indicators with X12 Claim Status codes to maximize your staff’s efficiency
Real Time Claim Status and Verification
Invicta Health Solutions delivers Real-time Claim Status access to 850+ payers nationwide including Medicare, Veterans Administration, most state Medicaid and HMOs, and all major commercial payers.
Real-Time Eligibility Checks
Invicta Health Solutions delivers Real-time Eligibility checks for more than 1,000 payers including Medicare, Veterans Administration, Medicaid and HMOs, and all major commercial and managed care payers.
- Real-time API or batch connectivity
- Identify and secure all available coverage options available to our clients’ uninsured / self-pay patients
- Expand coverage hours, resulting in increased time and attention dedicated to each patient
- Assist more patients in identifying all potential sources of payment for their health services, while maintaining a high standard of quality
- Find payment sources, enroll patients in programs for which they are eligible
- Manage all aspects of the financial claims process
- Create a positive experience for patients while also improving client cash collected and account receivables that would otherwise be categorized as bad debt
- No tedious payer credentialing requirements – a simple one-page signed authorization form is all we need
Real Time Claim Status and Verification
Invicta Health Solutions delivers Real-time Claim Status access to 850+ payers nationwide including Medicare, Veterans Administration, most state Medicaid and HMOs, and all major commercial payers.

- Real-time API or batch connectivity
- “Next Day” turn around response time for batches
- Flexible file exchange workflows for batch connectivity
- Complete the work overnight with viable responses to you the following morning
- File exchange delivery via custom-built SFTP just for you
- No tedious payer credentialing requirements – a simple one-page signed authorization form is all we need
- Add a custom field to your return file to facilitate automation or workflows for your internal workflow management system
- Crosswalk your EPIC billing indicators with X12 Claim Status codes to maximize your staff’s efficiency
Real-Time Eligibility Checks
Invicta Health Solutions delivers Real-time Eligibility checks for more than 1,000 payers including Medicare, Veterans Administration, Medicaid and HMOs, and all major commercial and managed care payers.

- Real-time API or batch connectivity
- Identify and secure all available coverage options available to our clients’ uninsured / self-pay patients
- Expand coverage hours, resulting in increased time and attention dedicated to each patient
- Assist more patients in identifying all potential sources of payment for their health services, while maintaining a high standard of quality
- Find payment sources, enroll patients in programs for which they are eligible
- Manage all aspects of the financial claims process
- Create a positive experience for patients while also improving client cash collected and account receivables that would otherwise be categorized as bad debt
- No tedious payer credentialing requirements – a simple one-page signed authorization form is all we need
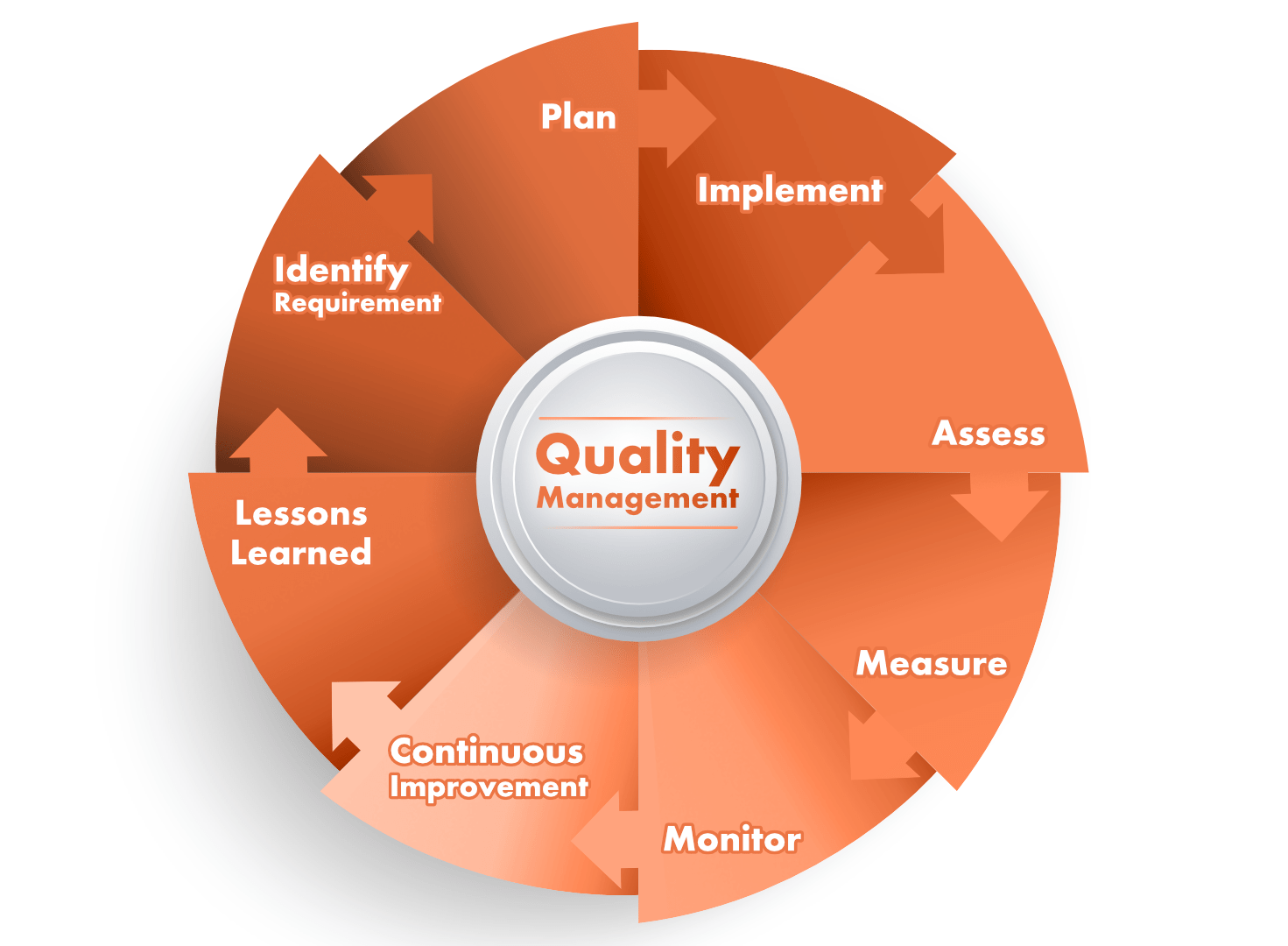
Quality Management
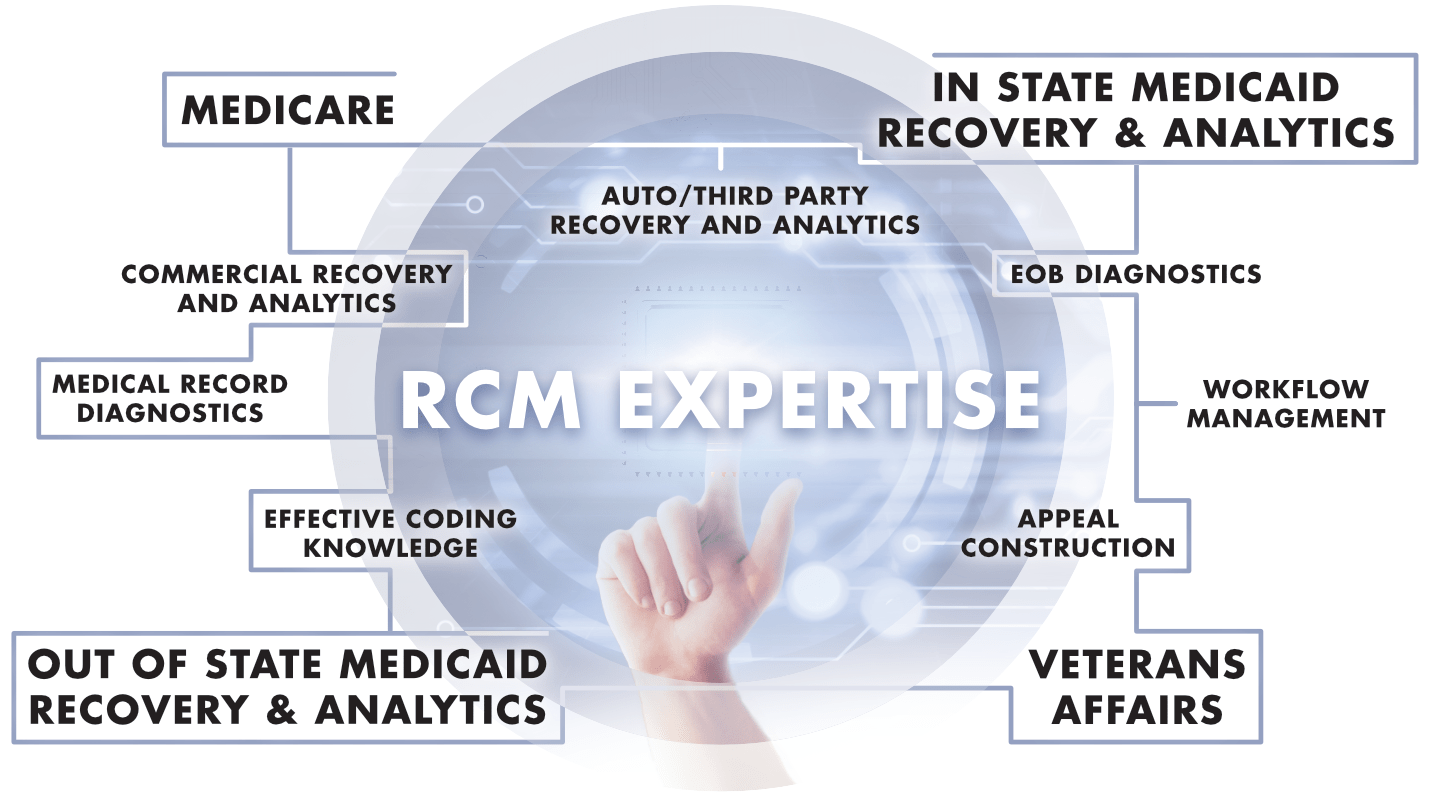
MEDICARE SOLUTIONS AND ANALYTICS
- Produce advanced analytics that drive pre- and post-bill management of Medicare Part A claim inventory
- Create improved performance of client’s largest payer category
- Receive in-depth analysis of top denial reason codes and revenue delayed or lost due to specific denials
- Track ongoing volumes of Medicare claim statuses such as:
• Return to Provider (RTP)
• Additional Documentation Required (ADR)
• Denials
• Suspense
• Payments
MEDICARE BENEFICIARY IDENTIFIER (MBI)
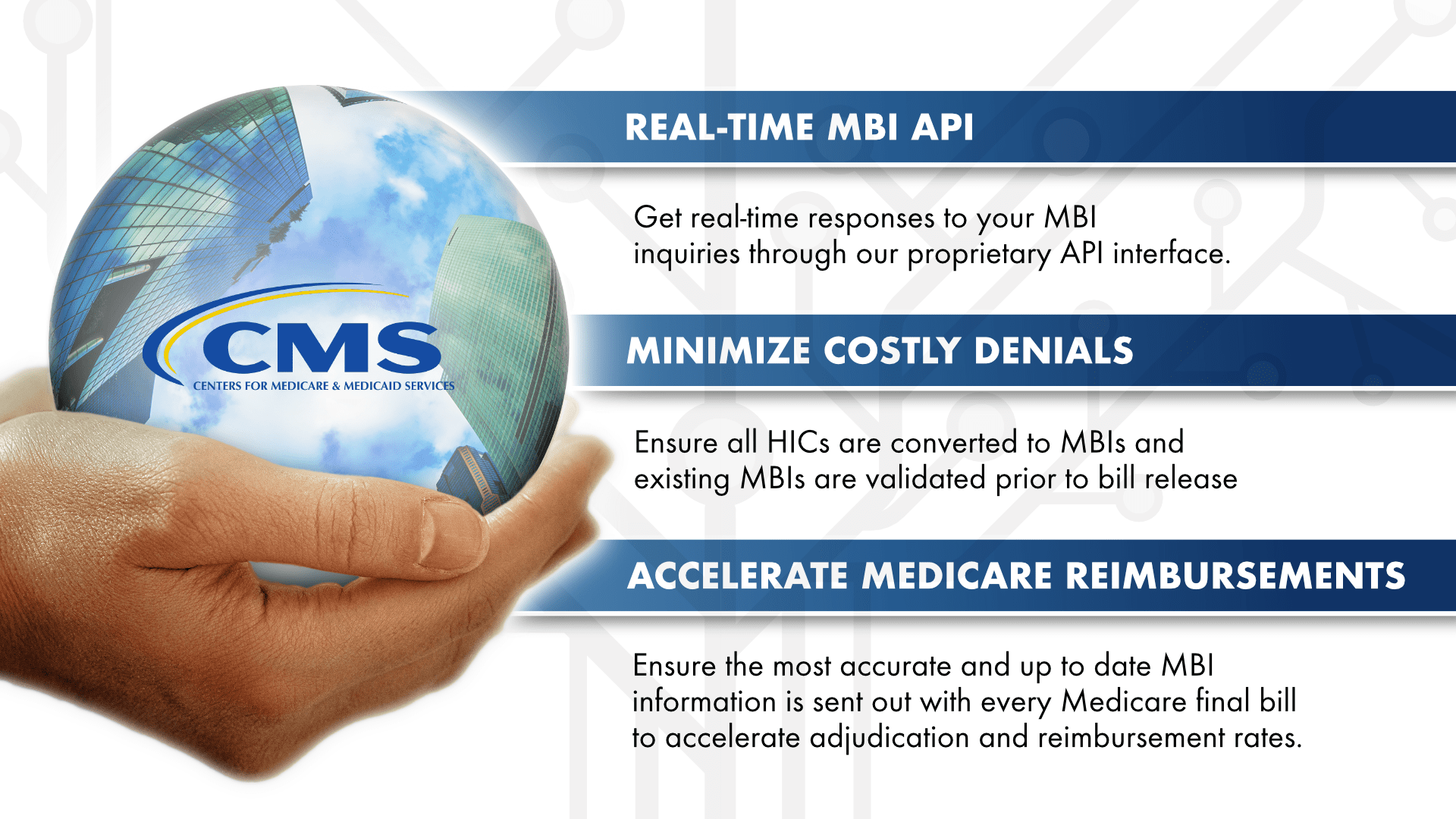
- Delivery of a proprietary solution that resolves Medicare eligibility data gaps as a result of ongoing regulatory changes
- Return MBI information from found Medicare coverage, as opposed to traditional redacted 271 responses
ROBOTIC PROCESS AUTOMATION (RPA)
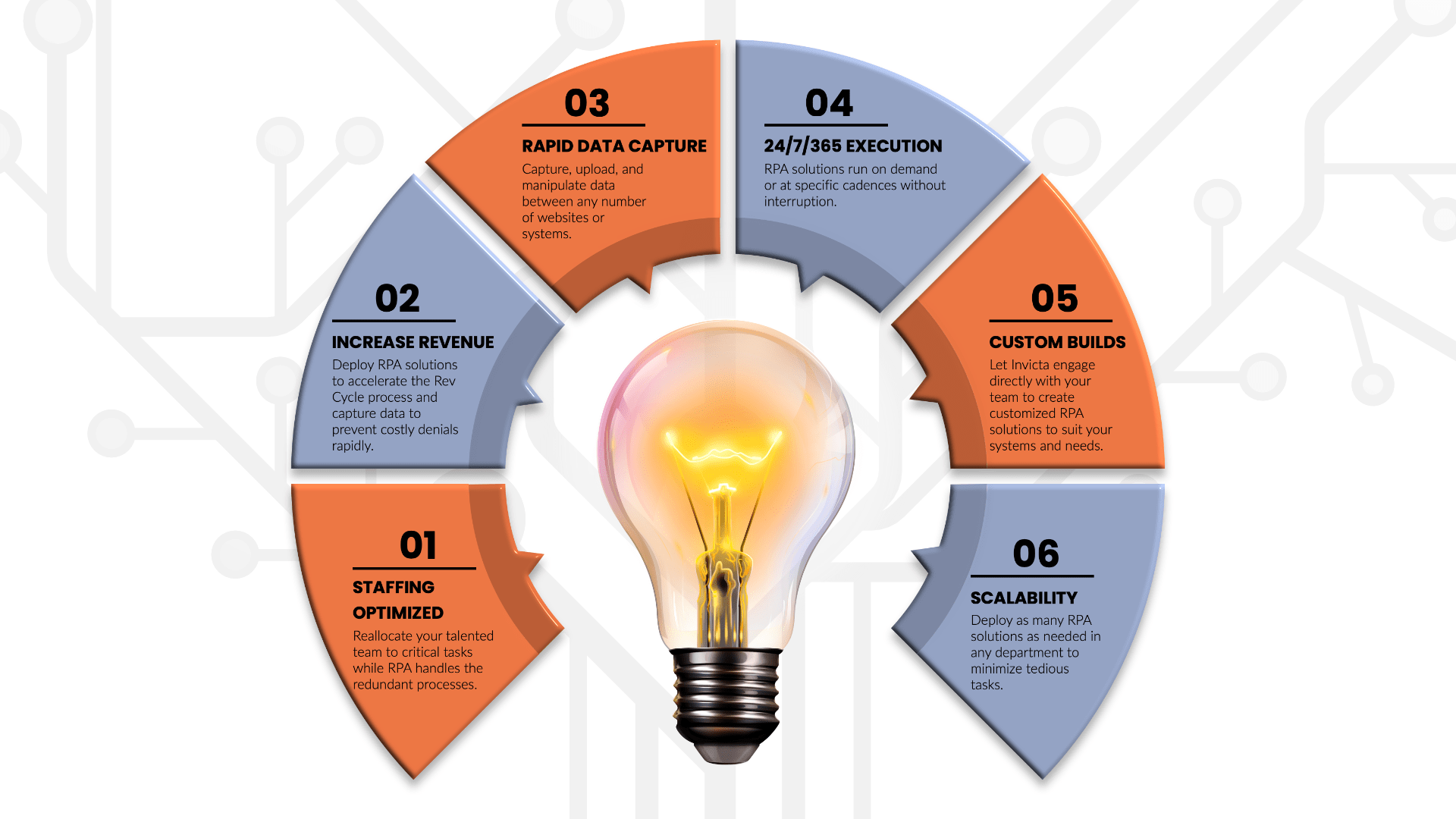
- EOS™ technology, which uses Robotic Process Automation, efficiently and accurately reviews each patient’s demographic and eligibility related information prior to submission
- Help you focus on human intervention for problematic and complex situations
INNOVATION AS A SERVICE

We utilize an “innovate and automate” approach to improve operational and financial performance for our clients. We align analytic solutions with superior customer service to process patient accounts, improving the reimbursement process and driving revenue acceleration for clients. Whether through our Technology Solutions or our Services, our organizational structure and technology-forward approach allows us to offer innovation as a service and a standard.
- Dedicated Innovation Development Team
• Revenue cycle management consultant
• Technology engineering consultant
• Innovation project manager - Remote Solution Hosting Option
• Manages all solution maintenance
• Provides in-depth analytic performance reports - On-site Team Hosting Option
• Dedicated on-site solution team stationed at facility
• Ongoing custom discovery, development, and deployment of solutions
innovation as a service
At Invicta, we constantly strive to redefine the standard of excellence in everything we do. We are open to ideas that challenge the conventional views and drive innovation. We believe that in order to stay relevant we must constantly improve with society’s changing needs.
We utilize an “innovate and automate” approach to improve operational and financial performance for our clients. We align analytic solutions with superior customer service to process patient accounts, improving the reimbursement process and driving revenue acceleration for clients. Whether through our Technology Solutions or our Services, our organizational structure and technology-forward approach allows us to offer innovation as a service and a standard.
- Dedicated Innovation Development Team
• Revenue cycle management consultant
• Technology engineering consultant
• Innovation project manager - Remote Solution Hosting Option
• Manages all solution maintenance
• Provides in-depth analytic performance reports - On-site Team Hosting Option
• Dedicated on-site solution team stationed at facility
• Ongoing custom discovery, development, and deployment of solutions