Out of state medicaid
Invicta offers clients the ultimate in trust, flexibility, and customization for Out of State Medicaid Billing.
- Handle all Medicaid claims – fee for service and managed care
- Manage all aspects of billing, collection, and provider enrollment
- Work the claim from beginning to end or wherever you would like us to fit in your process
- Dedicated, seasoned RCM team with decades of experience
- Robust reporting capabilities can include dollars by state, account status, and account status code
- No minimum number of accounts or account balance
- Minimal paperwork needed to begin, and we accept electronic or paper files
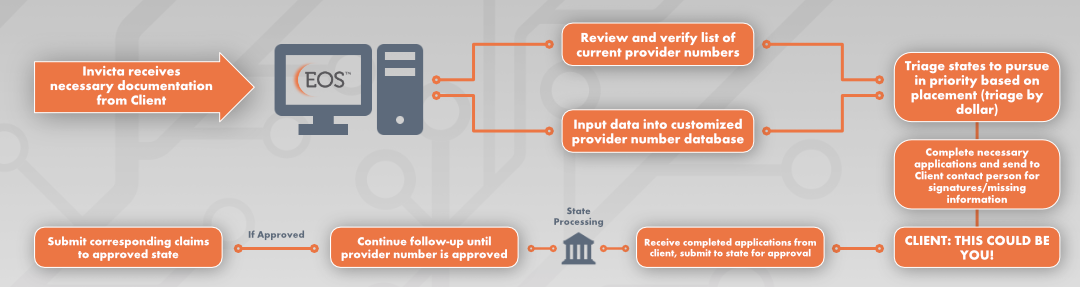
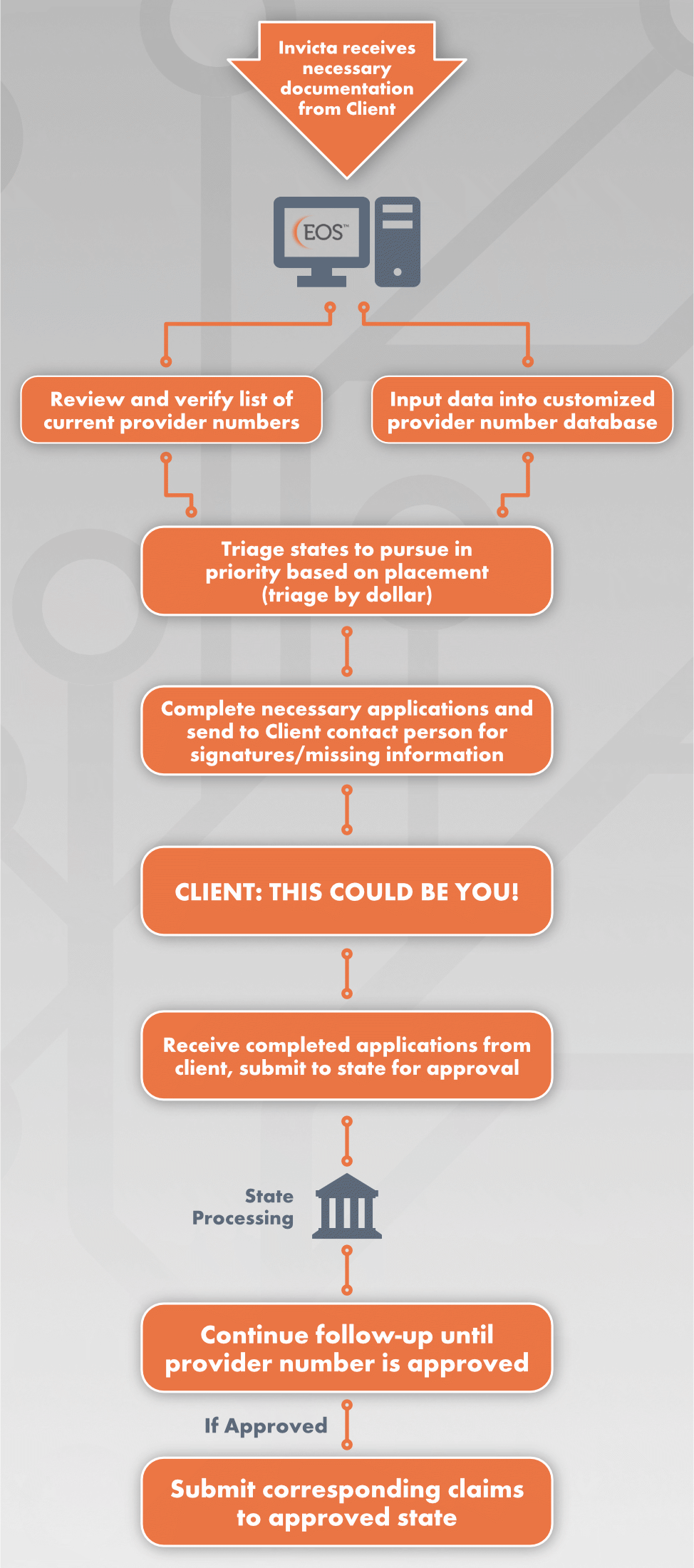
application Process
Provider number AUTOMATION and customization
- Provider Number Tracking by State
- Payer Demographics
- IP/OP Provider Number
- Timely Filing Deadlines
- Notes Field for Payer Requirements
- Effective/Expiration Tracking
- Automated Alert for Expiring IDs
- Active Total Charges Updated
- Maintain Prioritization in Workflow
- Interconnectivity to Invicta internal
- Clearinghouse
- Electronic Billing Available for All Payers with Supplied 837 File
Reporting
Package
- Monthly Invoicing
- Monthly Performance Reports
- Resolved Reports
- Electronic Notes Transmission
- Active Provider Number Reporting
- Ad Hoc Reporting Available
LEARN MORE




