Advanced technology and expertise to resolve clinical and technical denials
Advanced technology and expertise to resolve clinical and technical denials
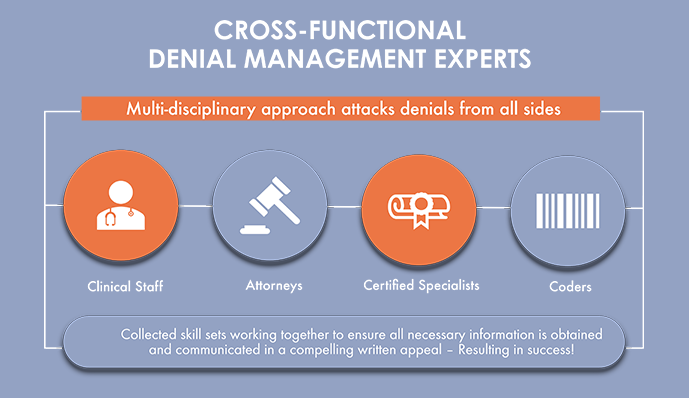
Denied claims are often the most disruptive portion of the revenue cycle process. Our cross-functional team of attorneys, clinicians, coders and reimbursement specialists work cohesively to craft appeals that result in approvals and subsequent payment.
Our EOS™ system identifies all tasks required for the submission of a successful appeal and automatically alerts the assigned staff member as deadlines approach. The combination of advanced technology and expert staff deliver a winning solution for denials for all payers and claim amounts.
Service philosophy
We are dedicated to the overall reduction of denials by utilizing a combination of advanced technology, expertise and superior workflows.
We understand our clients are providing medical care that is necessary and every payment, even low dollar, should receive reimbursement.
For a truly impactful solution, one must address both denial prevention and post bill resolution. We accomplish this objective through:
Utilizing our EOS technology solutions (pre and post bill) to reduce denials before they occur and efficiently address post bill occurrences;
Deploying a cross functional claims team of Attorneys, Clinicians, Medical Coders and Reimbursement Specialists;
Empowering our team which possess the skills and training to efficiently and aggressively manage each claim to maximize reimbursement;
Execution of superior workflows and proven processes resulting in improved efficiency and increased data accuracy.




