Disrupting Denial Management benefits Invicta Healthcare Clients and Patients
Denial Management is the process of investigating every unpaid claim a hospital receives from payers, identifying and preventing or correcting human error, and appealing to the insurance carrier. Sounds simple, doesn’t it? In fact, Denial Management is one of the most challenging and time-consuming processes in revenue cycle management services. We recently asked Invicta’s Chief Client Officer, Jude Crowell, to share his experiences with Denial Management in the field and to articulate what differentiates Invicta Health Solutions as a service provider for hospitals and health systems in this specialized discipline.
Why is Denial Management so difficult for organizations to successfully manage today?
At Invicta, we believe that hospitals and healthcare facilities should be reimbursed for the work they do, without hindrance and without delay. Recently, Becker’s Hospital Review published an article that quotes a recent survey of hospital executives, 30% of whom said they are seeing their average rate of denied insurance claims well above the historic average of 10%. You must remember that denials are simply a mathematical equation for the individuals reviewing the claim on the carrier side. As insurers refine their claim review process, they identify new ways to flag the claims. It’s just business. And the profit margins were tremendous for those businesses in 2020 when we began fighting COVID-19, while hospitals saw markedly reduced profits last year. With Medicare and managed care programs, we’ve also seen trends that show upticks in those denial management rates from their previous ones.
Hospitals, health systems and their doctors and nurses serve people. And their number one goal is to diagnose and treat the patients so they can return home. We don’t believe that service providers – like Invicta – or carriers should second-guess the treatment plans of qualified hospital personnel. Consequently, we are committed to supporting our clients with Denial Management services with robust integration of smart specialists and business intelligence.
What are the main reasons that valid claims are denied?
Human error is the first possible cause and it makes up nearly 50% of the cases, because people can make mistakes. When a patient receives services through a healthcare provider, their point of entry is most often with the friendly front of house team to complete registration and put them in queue. We provide real time claim status and real time eligibility checks for our clients, which can greatly reduce the error issue during the eligibility verification process. But for systems that don’t have our services and solutions in place, those front end verification processes can contain errors – often because time is of the essence and no system wants to deny or slow down appropriate services. We see this challenge quite a bit in cases of cancer and Emergency Room visits. Coding mistakes make up the roughly other half of the “human error” cases. Coding is a black and white environment. Human beings and healthcare services are full of gray. A hospital may be using an in-house team or contracting to a service provider than may likely be using contractors outside of the United States, who may be inexperienced with the insurance processes and the healthcare industry in general. This is where quality control KPIs come into play.
1
Human error is the first possible cause and it makes up nearly 50% of the cases, because people can make mistakes. When a patient receives services through a healthcare provider, their point of entry is most often with the friendly front of house team to complete registration and put them in queue. We provide real time claim status and real time eligibility checks for our clients, which can greatly reduce the error issue during the eligibility verification process. But for systems that don’t have our services and solutions in place, those front end verification processes can contain errors – often because time is of the essence and no system wants to deny or slow down appropriate services. We see this challenge quite a bit in cases of cancer and Emergency Room visits. Coding mistakes make up the roughly other half of the “human error” cases. Coding is a black and white environment. Human beings and healthcare services are full of gray. A hospital may be using an in-house team or contracting to a service provider than may likely be using contractors outside of the United States, who may be inexperienced with the insurance processes and the healthcare industry in general. This is where quality control KPIs come into play.
Disagreement over what is medically necessary for acute inpatient stays make up about 30 percent of the denials we see. In these cases, a medical expert working for the insurer reviews more claims than they can possibly manage and make quick judgements on how the provider could or should handle things differently. This is where it becomes challenging and requires the attention of clinicians and reimbursement specialists. Invicta has a seriously stacked team in place for this!
Disagreement over what is medically necessary for acute inpatient stays make up about 30 percent of the denials we see. In these cases, a medical expert working for the insurer reviews more claims than they can possibly manage and make quick judgements on how the provider could or should handle things differently. This is where it becomes challenging and requires the attention of clinicians and reimbursement specialists. Invicta has a seriously stacked team in place for this!
3
Clinical denials make up the rest of the denied claims in a provider’s inbox. Clinical validation denials are in essence a challenge to the provider’s clinical decisions, findings, and treatments. I want to repeat what I said earlier: This is where Invicta really shines. If you consider that 80-90 percent of denied claims are actually for insured individuals, imagine the difficulties faced by someone who is not insured. Our goal is to help our clients – many of whose patients are underinsured or uninsured – prevent mistakes on the front end and through coding. For example, the Medicare system has 5 levels of appeals: Redetermination by Medicare Contractor; Reconsideration by Independent Contractor; Office of Hearings and Appeals Decision; Medicare Appeals Council; and Federal District Court Review. In cases where a claim comes back denied due to a clinical validation, it often requires a 3rd, 4th, or (rare cases) 5th level of appeal.
3
Clinical denials make up the rest of the denied claims in a provider’s inbox. Clinical validation denials are in essence a challenge to the provider’s clinical decisions, findings, and treatments. I want to repeat what I said earlier: This is where Invicta really shines. If you consider that 80-90 percent of denied claims are actually for insured individuals, imagine the difficulties faced by someone who is not insured. Our goal is to help our clients – many of whose patients are underinsured or uninsured – prevent mistakes on the front end and through coding. For example, the Medicare system has 5 levels of appeals: Redetermination by Medicare Contractor; Reconsideration by Independent Contractor; Office of Hearings and Appeals Decision; Medicare Appeals Council; and Federal District Court Review. In cases where a claim comes back denied due to a clinical validation, it often requires a 3rd, 4th, or (rare cases) 5th level of appeal.
What are the toughest denied claims to manage?
Sadly, the most challenging and frequently denied claims revolve around cancer, Emergency Room services, and end of life. We understand that for the patient, hospital, and physicians, these are the costliest and most time-sensitive claims. We want people to be appropriately insured so that they can be pro-active in managing their own health and participating in preventative healthcare programs. As we all know, cancer doesn’t care. Accidents happen. And end of life requires expensive care.
What are the ingredients in Invicta’s service philosophy?
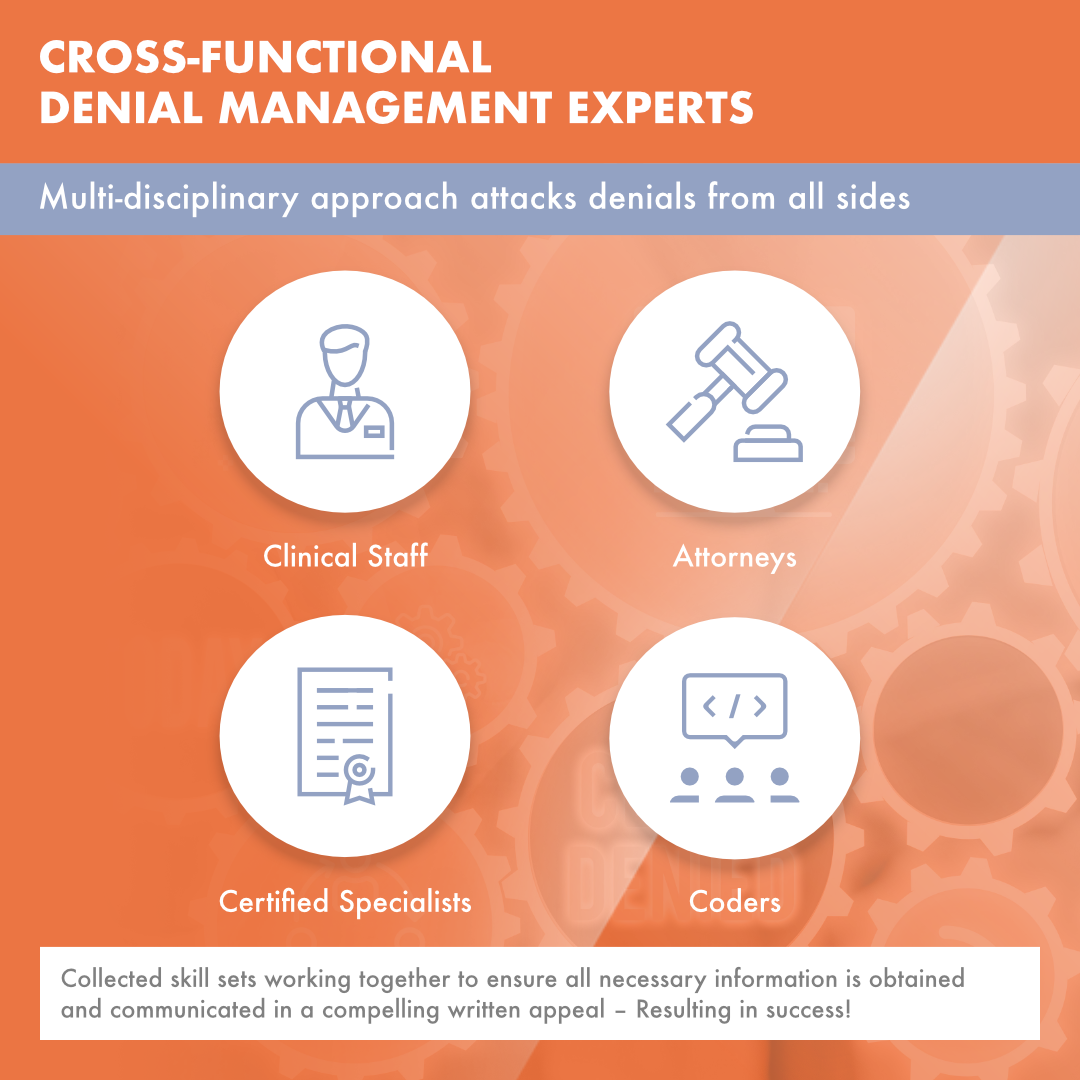
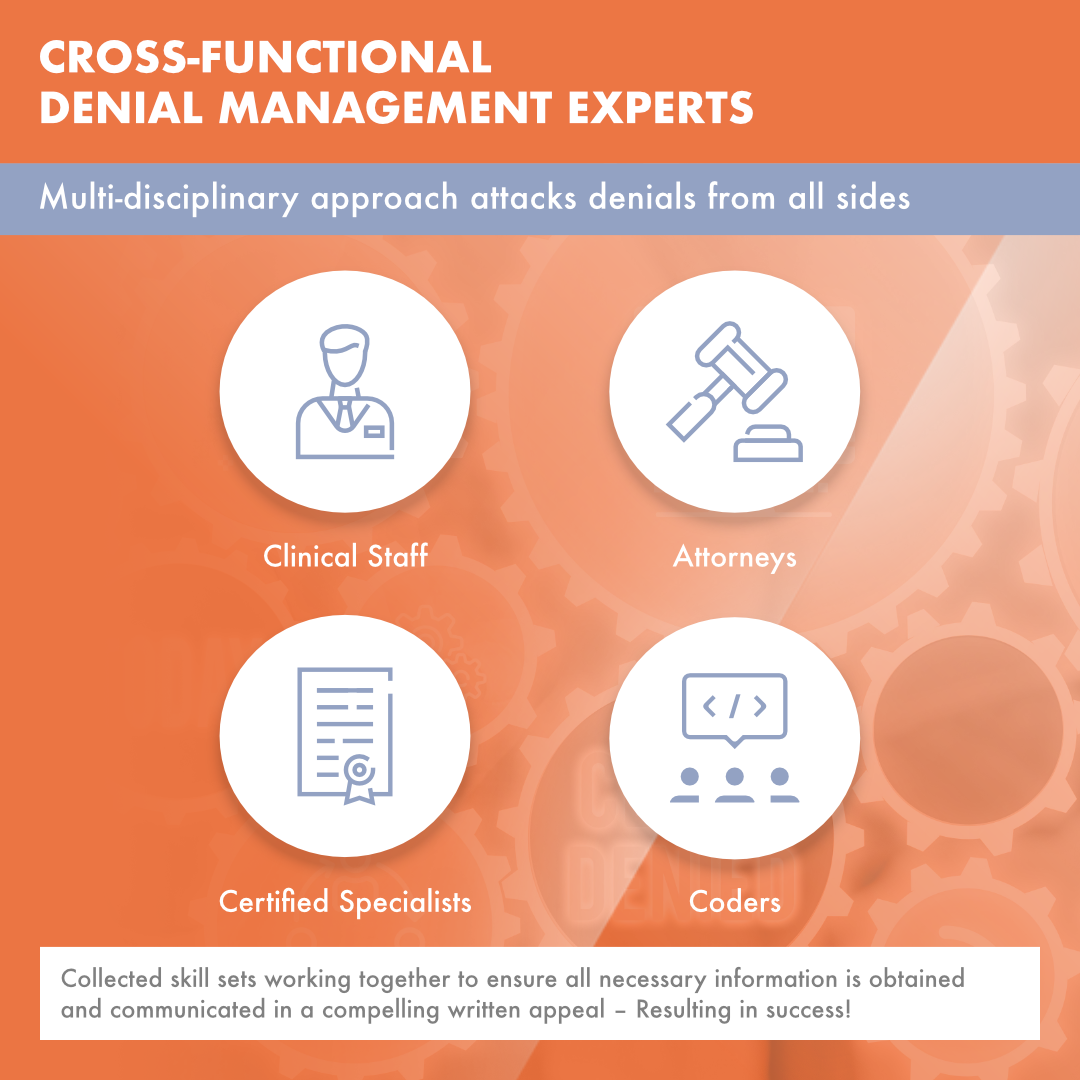
Great question! I wish more providers asked this question when making comparisons between internal teams, outside service providers and/or hybrid models. We help our clients achieve an overall reduction of denials by utilizing advanced technology, expertise, and superior workflows. We use an efficient and aggressive approach for denial management and appeals. Our cross-functional team of attorneys, clinicians, coders, and reimbursement specialists work cohesively to craft appeals that result in approvals and subsequent payment. Our EOS™ system identifies all tasks required for the submission of a successful appeal and automatically alerts the assigned staff member as deadlines approach. The combination of advanced technology and expert staff deliver a winning solution for denials for all payers and claim amounts.
We can help our clients address both pre-bill (prevention) and post bill resolution by:
- Utilizing our EOS technology solutions (pre and post bill) to reduce denials before they occur and efficiently address post bill occurrences;
- Deploying a cross functional claims team of Attorneys, Clinicians, Medical Coders and Reimbursement Specialists;
- Empowering our team which possess the skills and training to efficiently and aggressively manage each claim to maximize reimbursement;
- Execution of superior workflows and proven processes resulting in improved efficiency and increased data accuracy.
What is the Invicta value proposition for handling Denial Management?
Our people, processes and technology make the difference. Plainly speaking, we want providers to be equitably reimbursed and we want to help fix what may be wrong in their claims submission process. We can quickly and easily conduct a root cause analysis, mitigate the risks of future denials, and help our clients get paid faster. We can “automate and innovate“ the process for low balance claims, and we embrace the challenges of the high dollar claims that can overwhelm a healthcare provider’s team. We understand that our clients are providing medical care that is necessary: Every payment, even low dollar ones, should receive reimbursement.
If you’d like to bring Invicta’s Denial Management services to your organization, contact us at info@invictahs.com for more information.
LEARN MORE




